Complementary, Alternative, or Integrative Health: What’s In a Name?

We’ve all seen the words “complementary,” “alternative,” and “integrative,” but what do they really mean?
This fact sheet looks into these terms to help you understand them better and gives you a brief picture of the mission and role of the National Center for Complementary and Integrative Health (NCCIH) in this area of research. The terms “complementary,” “alternative,” and “integrative” are continually evolving, along with the field, but the descriptions of these terms below are how we at the National Institutes of Health currently define them.
Complementary Versus Alternative
According to a 2012 national survey, many Americans—more than 30 percent of adults and about 12 percent of children—use health care approaches that are not typically part of conventional medical care or that may have origins outside of usual Western practice. When describing these approaches, people often use “alternative” and “complementary” interchangeably, but the two terms refer to different concepts:
- If a non-mainstream approach is used together with conventional medicine, it’s considered “complementary.”
- If a non-mainstream approach is used in place of conventional medicine, it’s considered “alternative.”
Most people who use non-mainstream approaches also use conventional health care.
In addition to the terms complementary and alternative, you may also hear the term “functional medicine.” This term sometimes refers to a concept similar to integrative health (described below), but it may also refer to an approach that more closely resembles naturopathy (a medical system that has evolved from a combination of traditional practices and health care approaches popular in Europe during the 19th century).
Integrative Health
Integrative health brings conventional and complementary approaches together in a coordinated way. Integrative health also emphasizes multimodal interventions, which are two or more interventions such as conventional health care approaches (like medication, physical rehabilitation, psychotherapy), and complementary health approaches (like acupuncture, yoga, and probiotics) in various combinations, with an emphasis on treating the whole person rather than, for example, one organ system. Integrative health aims for well-coordinated care among different providers and institutions by bringing conventional and complementary approaches together to care for the whole person.
The use of integrative approaches to health and wellness has grown within care settings across the United States. Researchers are currently exploring the potential benefits of integrative health in a variety of situations, including pain management for military personnel and veterans, relief of symptoms in cancer patients and survivors, and programs to promote healthy behaviors.
What is whole person health?
Whole person health refers to helping individuals, families, communities, and populations improve and restore their health in multiple interconnected domains—biological, behavioral, social, environmental—rather than just treating disease. Research on whole person health includes expanding the understanding of the connections between these various aspects of health, including connections between organs and body systems.
Integrative Approaches for Pain Management for Military Personnel and Veterans
- Chronic pain is a common problem among active-duty military personnel and veterans. NCCIH, the U.S. Department of Veterans Affairs, and other agencies are sponsoring research to see whether integrative approaches can help. For example:
- An NCCIH-funded study is developing an innovative, collaborative treatment model involving chiropractors, primary care providers, and mental health providers for veterans with spine pain and related mental health conditions.
- Other NCCIH-funded studies are testing the effects of adding mindfulness meditation, self-hypnosis, or other complementary approaches to pain management programs for veterans. The goal is to help patients feel and function better and reduce their need for pain medicines that can have serious side effects.
- For more information on pain management for military personnel and veterans, see NCCIH’s Complementary Health Practices for U.S. Military, Veterans, and Families webpage.
Integrative Approaches for Symptom Management in Cancer Patients and Survivors
- Cancer treatment centers with integrative health care programs may offer services such as acupuncture and meditation to help manage symptoms and side effects for patients who are receiving conventional cancer treatment. Although research on the potential value of these integrative programs is in its early stages, some studies have had promising results. For example, NCCIH-funded research has suggested that:
- Massage therapy may lead to short-term improvements in pain and mood in patients with advanced cancer.
- Yoga may relieve the persistent fatigue that some women experience after breast cancer treatment, according to the results of a preliminary study.
- Tai chi or qigong have shown promise for managing symptoms such as fatigue, sleep difficulty, and depression in cancer survivors.
- For more information, see NCCIH’s fact sheet on cancer.
Complementary Health Approaches
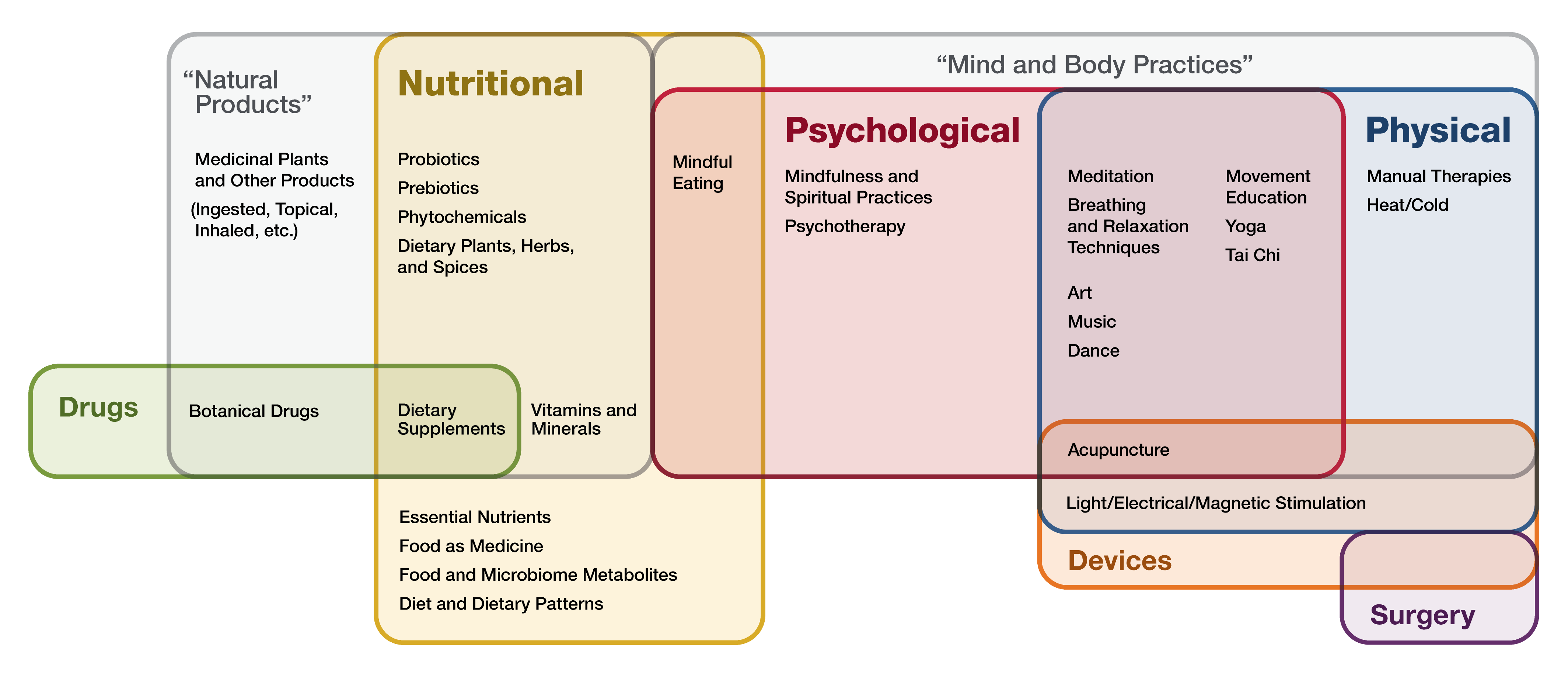
Complementary approaches can be classified by their primary therapeutic input (how the therapy is taken in or delivered), which may be:
- Nutritional (e.g., special diets, dietary supplements, herbs, and probiotics)
- Psychological (e.g., mindfulness)
- Physical (e.g., massage, spinal manipulation)
- Combinations such as psychological and physical (e.g., yoga, tai chi, acupuncture, dance or art therapies) or psychological and nutritional (e.g., mindful eating)
Nutritional approaches include what NCCIH previously categorized as natural products, whereas psychological and/or physical approaches include what was referred to as mind and body practices.
Nutritional Approaches
These approaches include a variety of products, such as herbs (also known as botanicals), vitamins and minerals, and probiotics. They are widely marketed, readily available to consumers, and often sold as dietary supplements.
According to the 2012 National Health Interview Survey (NHIS), which included a comprehensive survey on the use of complementary health approaches by Americans, 17.7 percent of American adults had used a dietary supplement other than vitamins and minerals in the past year. These products were the most popular complementary health approach in the survey. (See chart.) The most commonly used nonvitamin, nonmineral dietary supplement was fish oil.
Researchers have done large, rigorous studies on a few dietary supplements, but the results often showed that the products didn’t work for the conditions studied. Research on others is in progress. While there are indications that some may be helpful, more needs to be learned about the effects of these products in the human body, and about their safety and potential interactions with medicines and other natural products.
Psychological and Physical Approaches
Complementary physical and/or psychological approaches include tai chi, yoga, acupuncture, massage therapy, spinal manipulation, art therapy, music therapy, dance, mindfulness-based stress reduction, and many others. These approaches are often administered or taught by a trained practitioner or teacher. The 2012 NHIS showed that yoga, chiropractic and osteopathic manipulation, and meditation are among the most popular complementary health approaches used by adults. According to the 2017 NHIS, the popularity of yoga has grown dramatically in recent years, from 9.5 percent of U.S. adults practicing yoga in 2012 to 14.3 percent in 2017. The 2017 NHIS also showed that the use of meditation increased more than threefold from 4.1 percent in 2012 to 14.2 percent in 2017.
Other psychological and physical approaches include relaxation techniques (such as breathing exercises and guided imagery), qigong, hypnotherapy, Feldenkrais method, Alexander technique, Pilates, Rolfing Structural Integration, and Trager psychophysical integration.
Research findings suggest that several psychological and physical approaches, alone or in combination, are helpful for a variety of conditions. A few examples include the following:
- Acupuncture may help ease types of pain that are often chronic, such as low-back pain, neck pain, and osteoarthritis/knee pain. Acupuncture may also help reduce the frequency of tension headaches and prevent migraine headaches.
- Meditation may help reduce blood pressure, symptoms of anxiety and depression, and symptoms of irritable bowel syndrome and flare-ups in people with ulcerative colitis. Meditation may also benefit people with insomnia.
- Tai chi appears to help improve balance and stability, reduce back pain and pain from knee osteoarthritis, and improve quality of life in people with heart disease, cancer, and other chronic illnesses.
- Yoga may benefit people’s general wellness by relieving stress, supporting good health habits, and improving mental/emotional health, sleep, and balance. Yoga may also help with low-back pain and neck pain, anxiety or depressive symptoms associated with difficult life situations, quitting smoking, and quality of life for people with chronic diseases.
The amount of research on psychological and physical approaches varies widely depending on the practice. For example, researchers have done many studies on acupuncture, yoga, spinal manipulation, and meditation, but there have been fewer studies on some other approaches.
Other Complementary Health Approaches
Some complementary approaches may not neatly fit into either of these groups—for example, the practices of traditional healers, Ayurvedic medicine, traditional Chinese medicine, homeopathy, naturopathy, and functional medicine.
NCCIH’s Role
NCCIH is the Federal Government’s lead agency for scientific research on complementary and integrative health approaches.
NCCIH’s Mission and Vision
The mission of NCCIH is to determine, through rigorous scientific investigation, the fundamental science, usefulness, and safety of complementary and integrative health approaches and their roles in improving health and health care.
NCCIH’s vision is that scientific evidence informs decision making by the public, by health care professionals, and by health policymakers regarding the integrated use of complementary health approaches in a whole person health framework.
For More Information
NCCIH Strategic Plan
NCCIH’s current strategic plan, Strategic Plan FY 2021–2025: Mapping a Pathway to Research on Whole Person Health, presents a series of goals and objectives to guide us in determining priorities for future research on complementary health approaches.
NCCIH Clearinghouse
The NCCIH Clearinghouse provides information on NCCIH and complementary and integrative health approaches, including publications and searches of Federal databases of scientific and medical literature. The Clearinghouse does not provide medical advice, treatment recommendations, or referrals to practitioners.
Toll-free in the U.S.: 1-888-644-6226
Telecommunications relay service (TRS): 7-1-1
Website: https://www.nccih.nih.gov
Email: info@nccih.nih.gov (link sends email)
This publication is not copyrighted and is in the public domain. Duplication is encouraged.
NCCIH has provided this material for your information. It is not intended to substitute for the medical expertise and advice of your health care provider(s). We encourage you to discuss any decisions about treatment or care with your health care provider. The mention of any product, service, or therapy is not an endorsement by NCCIH.